Cases of monkeypox have risen around the D.C. region in recent weeks, but local public health departments’ responses to the emergence are varied, with some jurisdictions vaccinating only close contacts and others opening up appointments more broadly to communities disproportionately impacted. Throughout the region, and the country, vaccine supply is limited.
As of Friday, July 8, D.C. reported 60 cases total – up significantly from the seven cases reported initially on June 24. Maryland has reported 14 cases, while Virginia has reported 23, with 21 of those cases coming from the Northern Virginia region. Across the U.S., 700 cases have been reported, with the most occurring in California and New York. Experts anticipate more cases because the atypical symptoms of this strain of monkeypox has led to some initial misdiagnoses.
Monkeypox, a disease endemic to countries in Central and West Africa, emerged in the U.S. in mid-May. It’s in the Orthopoxvirus genus, which includes the virus that causes smallpox, which was officially eradicated in the 1980s.
Initial symptoms typically include a fever, muscle aches, and fatigue, and within a few days, a rash emerges. According to the Centers for Disease Control and Prevention, monkeypox spreads through close contact with an infectious rash, scabs, or bodily fluids, or through prolonged face-to-face contact, like kissing or sex. While the virus can spread to anyone, the current outbreak is occurring most commonly in men who have sex with men.
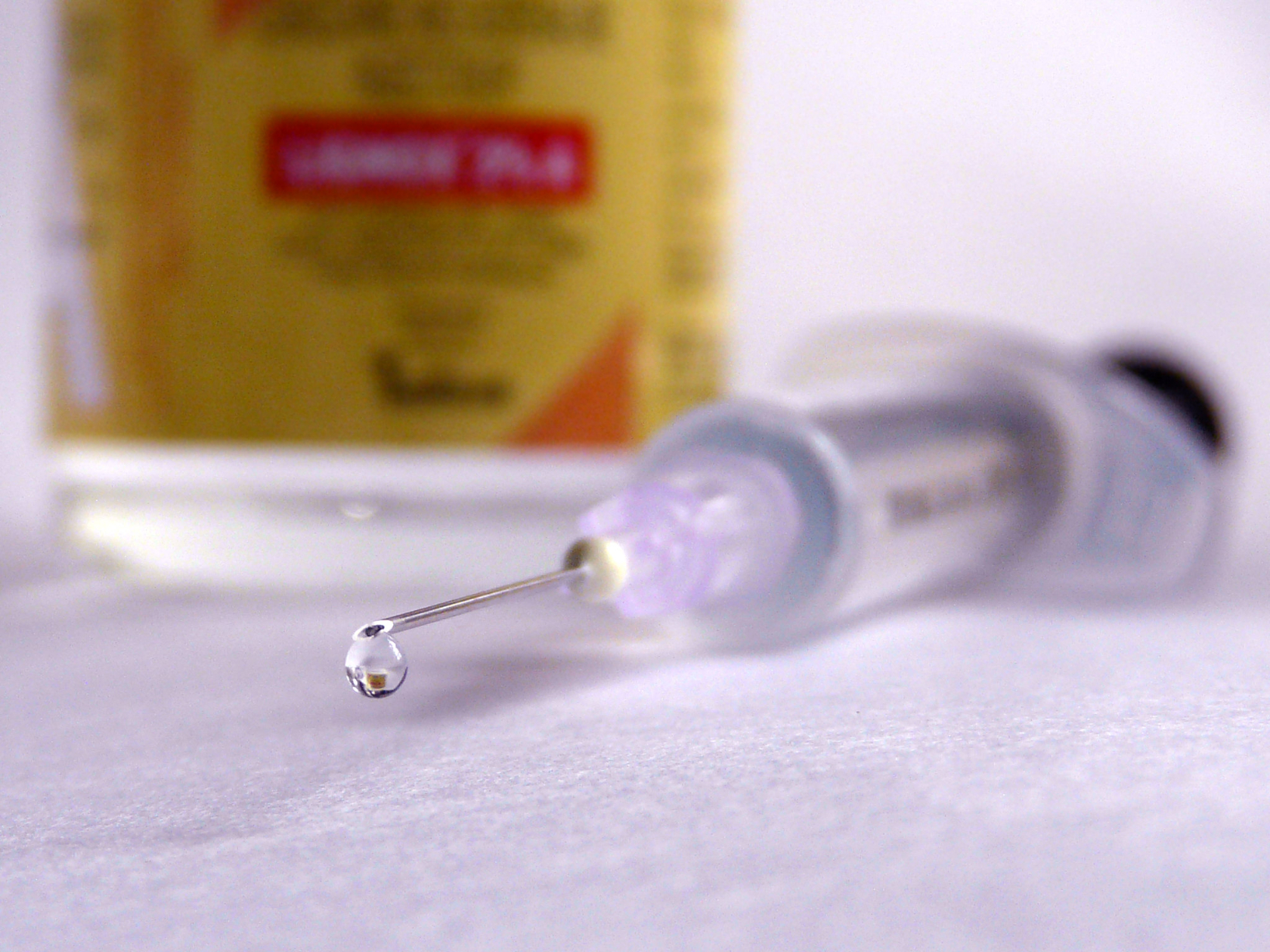
While the virus causes flu-like symptoms similar to COVID-19, it’s nowhere near as contagious – plus, given its similarity to smallpox, epidemiologists already know a lot about the illness and how to treat it. There is no specific treatment for a monkeypox infection, but antiviral drugs and vaccines developed to protect against smallpox are being used to both treat and prevent monkeypox cases.
In June, the federal government announced a plan to provide a vaccine for monkeypox to the states – but so far, administration in the region is limited and spotty.
The U.S. Department of Health and Human Services began sending doses of the JYNNEOS monkeypox vaccine to states in late June, with quantities based on requests from jurisdictions and supply restrictions. The federal government also has a second vaccine, ACAM2000, which has been FDA-approved to treat smallpox. While there is a greater quantity of ACAM2000 than JYNNEOS available, it is not recommended for everyone due to significant side effects.
On June 27, D.C. opened a limited number of vaccine appointments to a select population of residents. According to the city, the vaccine appointments are available to anyone over the age of 18, who meets the following criteria:
- Gay, bisexual, and other men 18 and older who have sex with men and have had multiple or anonymous sexual partners in the last 14 days); or
- Transgender women and nonbinary persons assigned male at birth who have sex with men; or
- Sex workers (of any sex); or
- Staff (of any sex) at establishments where sexual activity occurs (e.g., bathhouses, saunas, sex clubs)
Just 15 minutes after appointment slots opened on June 27, all 300 were booked up.
A similar scene played out this week, when DC Health tweeted at 10:00 a.m. on Tuesday that at 1:00 p.m. that afternoon, additional appointments were opening for Wednesday, Friday, and next Monday. Six minutes later, all 480 appointments were filled.
According to a statement from HHS Assistant Secretary for Preparedness and Response Dawn O’Connell, the department is working to “deliver vaccine [to states] as quickly as we can while we maintain a focus on fair and equitable distribution nationwide.” In the latest round of shipments on July 1, D.C. was allocated 1,206 doses, and on Thursday, July 7, HHS announced that an additional 144,000 JYNNEOS doses would be shipped out to states on July 11.
DC Health spokespeople did not return multiple requests for comment from DCist/WAMU about how, outside of Twitter, the department is making at-risk residents aware of vaccine availability. Neil Sehgal, a public health professor at the University of Maryland, is concerned that the city’s current plan for monkeypox vaccine distribution is breeding the same equity issued that beleaguered D.C.’s COVID-19 vaccine rollout.
“I don’t mean to over-compare COVID-19 and monkeypox, but I think both of these have touched on some of the weaknesses in our healthcare system and how they may precipitate inequity,” Sehgal says. “There are people in [D.C.’s] eligible group that don’t have the ability to refresh a browser at one in the afternoon, and some of those may be the people in greatest need, or who would benefit most, or who were highest risk.”
During a call with DCist/WAMU last week regarding the end of the city’s COVID-19 contact tracing program, DC Health senior officer Patrick Ashley said the department has shifted staffing around to handle investigation and contract tracing of monkeypox cases, but spokespeople for DC Health have not provided a more detailed plan for containing the outbreak.
“[Investigators] do follow up right now, with any monkeypox case, to understand where they might have been exposed, what sort of symptoms they have, who their contacts were, and then work with those contacts to get them in to either get tested or provide vaccination,” Ashley said last week.
While he notes D.C. is constricted by the amount of vaccine provided by the federal government, Sehgal says given D.C.’s current caseload per capita, it’s important that the health department work with LGBTQ+ community organizations and health providers to make resources and vaccines available to those potentially exposed or in close contact – especially those who cannot refresh a webpage on a weekday afternoon to book an appointment. Patrick Ashley of DC Health told DCist/WAMU on Friday that the agency so far has had two calls with local LGBTQ+ health providers. According to Ashley, there are not currently enough vaccine doses to provide them directly to health providers.
“What I do think is that the strategy so far of allocating vaccine appointments has favored people who are eligible, but also privileged,” Sehgal says.
Meanwhile, unlike D.C.’s open-appointment system, in Maryland and Virginia, doses of the monkeypox vaccine are currently reserved for individuals who have been exposed to a probable or confirmed case of monkeypox via contact tracing by the states’ health departments.
Larry Hill, a spokesperson for Virginia’s Department of Health, says that the state plans to offer the vaccine to additional high-risk individuals as supply from the federal government increases. Within the next week, according to Hill, VDH intends to host a small number of vaccine clinics targeting specific populations, including people who have multiple sex partners or anonymous sex partners, or who have attended events where an exposure occurred. To date, VDH has received 500 doses of the JYNNEOS vaccine.
Maryland is taking a similar approach: local health departments are administering the vaccine to individuals who have been in close contact with confirmed cases, according to a spokesperson for the state’s health department.
Mary Anderson, a spokesperson for Montgomery County, says that while Maryland Department of Health is taking the lead on the monkeypox response, the county health department has received a limited number of vaccine doses, which will be reserved right now for potentially-exposed individuals. Anderson says that so far, the county has only provided “a couple” of vaccines to close contacts of someone that was exposed to the virus, and the county will expand eligibility to more high-risk groups at the direction of federal supply and MDH guidelines.
Sehgal says that based on the number of cases in Maryland – nine currently, although that could be an undercount – their reserved vaccination plan makes sense. When there are a fairly small number of cases of a virus in a relatively large population, a strategy called “ring vaccination” is deployed to contain the spread – essentially, all close contacts of a confirmed case are vaccinated in order to mitigate any further spread.
“That ring vaccination strategy was effective during smallpox and under most epidemiologic conditions when you don’t meet this threshold of transmission, especially asymptomatic transmission, broadly in a population,” Sehgal says. “Maryland’s approach is pretty reasonable.”
It’s also likely, Sehgal says, that the region – and the rest of the country – isn’t testing enough, (much like in the early days of the COVID-19 pandemic) so current caseloads are likely an undercount. The country is still in an “exponential growth” phase, according to Sehgal.
“I do expect the number to climb, not just in the District, I expect to see a climb in New York, California, Massachusetts,” he says. “I’m prone to anxiety generally, but I don’t think it’s panic-inducing at this point. I do think it’s cause for alarm…but we have a reasonable understanding of how transmission is occurring, and so certainly the additional precautions to limit spread, especially in the groups that are at greatest risk, is warranted right now.”
 Colleen Grablick
Colleen Grablick