Shortly after the region saw coronavirus case counts drop to record-breaking lows, infections are on the rise again in the D.C. area.
Experts attribute the rise to myriad factors occurring at once: vaccination rates plateaued, masks requirements dropped, businesses reopened fully, summer gatherings picked up, and a new, more transmissible Delta variant is spreading across the country.
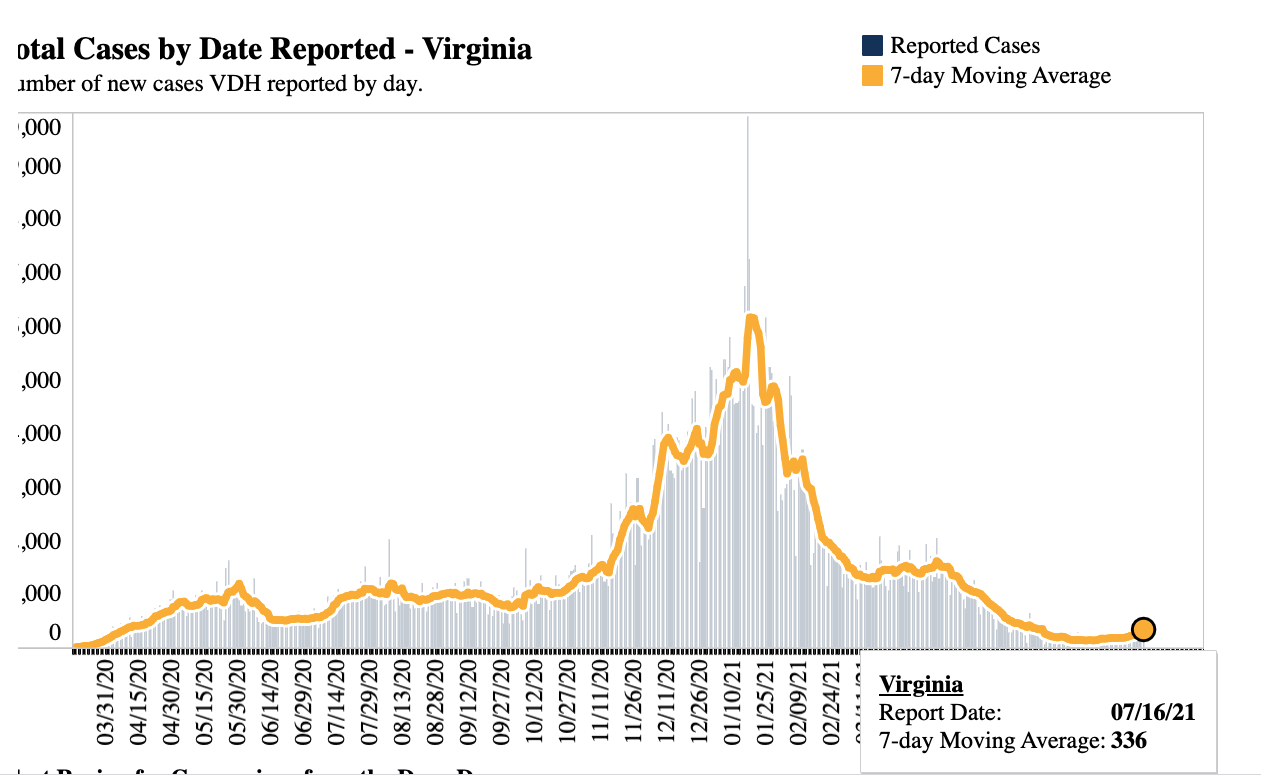
According to the Washington Post’s regional tracker, D.C. saw a 160% increase in new cases over the past seven days, while Maryland recorded a 72% increase, and Virginia 63%. The total seven-day average of new cases in all three jurisdictions has risen from 246 on June 16, to 454 as of July 16. Still, that remains well below the number recorded during the surge this past January, when the regional average topped 8,000 new cases a day.
“We’re encouraged that our surrounding jurisdictions in the DMV have experienced as much success with vaccination as we have so we feel pretty good about where we are in the city, yet we know that the virus is still out there in the world,” said D.C. Mayor Muriel Bowser when asked about the slight increase in infections during a press conference on Thursday. “We will continue to monitor it very closely and if we have some concerns we’ll report that.”
Since late May, D.C.’s average rate of daily cases per 100,000 residents has stayed below 5 – the threshold that indicates minimal community spread. In late June, the metric dropped to its lowest ever, around 1.3. But in the first weeks of July, that rate has ticked up slightly, and stands just above 3 as of July 13.
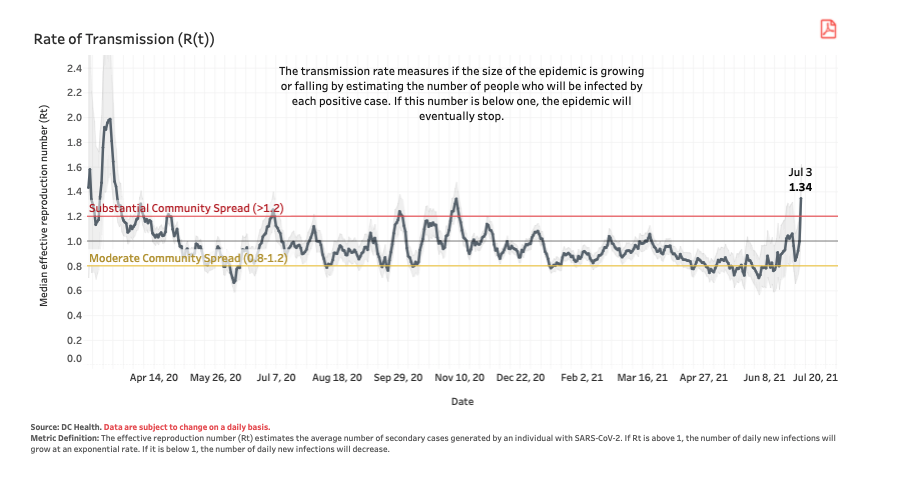
Perhaps more notable is the change in the city’s rate of transmission, a metric that measures the size of a pandemic in an area by estimating how many people are infected by one positive case. D.C.’s rate of transmission, as of July 3, is 1.34 — the highest recorded rate since November 2020. Any rate of transmission greater than 1.2 indicates substantial community spread. COVID-19-related hospitalizations in the city have remained stable, with the latest recorded data on July 11 showing a continued decline in the percentage of hospitalizations due to the virus.
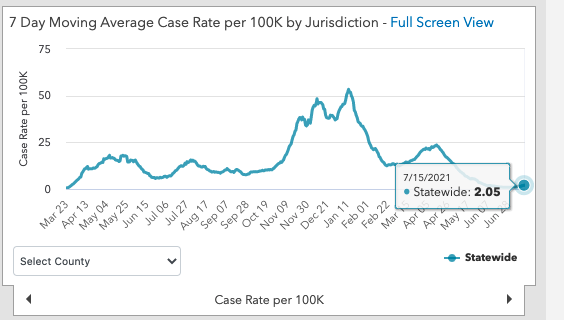
Maryland has also seen an increase in its average daily case rate per 100,000 residents; in the last days of June, the metric hovered below 1, and has now crept up near 2. Regionally, Montgomery County’s average case rate trend looks similar to that of the state, while Prince George’s County has seen a larger increase. The county’s average daily case rate per 100,000 is now over 3, while it dipped below 1 in late June.
In Virginia, the average daily case rate per 100,000 reached 3.62 as of July 15, the highest that metric has been since late May. While the seven-day average of new cases dipped as low as 177 on June 30, that metric increased to 336 as of July 16 – a number also not recorded since late May. More optimistically, both Virginia and Maryland have not reported increases in hospitalizations yet.
While it’s too early to determine whether the region’s slight increase in cases will sustain in the coming months, there’s one thing public health officials say can definitively prevent it from continuing: vaccinations.
“I really hope that we can intervene with vaccines to stop that from happening, and that’s really when it’s going to take,” said Jennifer Nuzzo, an epidemiologist and senior scholar at the Johns Hopkins Center for Health Security. “Vaccines is how we end this thing — it doesn’t mean it goes away, but we stop worrying about it as a perpetual threat.”
With all of the region’s coronavirus restrictions and mask guidances fully ended, and the more-transmissible Delta variant spreading throughout the region, Nuzzo underscores the most effective way to eliminate future spikes is to increase vaccination uptake. In the month of June, all Maryland residents who died of the virus were unvaccinated, and unvaccinated residents accounted for 95% of new COVID cases. Similarly in Virginia, a new dashboard shows that the virus is almost exclusively affecting partially vaccinated or unvaccinated individuals.
“It’s taking advantage of the unvaccinated,” Nuzzo says. “Delta would be less of a threat if we were able to vaccinate all the adults who are eligible for vaccination, but the fact that we haven’t has enabled delta to take root and to spread as quickly as it has.”
Nationally, the Delta variant made up nearly 60% of all new COVID-19 cases reported from June 20 to June 3, according to the Center for Disease Control. Virginia has recorded 158 cases of the variant as of June 16, with 39 of those cases coming from Northern Virginia. Maryland’s Department of Health recorded 90 cases of the Delta variant as of July 12, and a spokesperson tells DCist in an emailed statement that “the proportion of cases that are caused by Delta is increasing substantially, and seems likely to replace Alpha as the most common lineage in Maryland.”
D.C. Health does not publish data on variant cases and did not immediately return DCist’s request for comment, but the Washington Post reported that the city has sequenced every positive case sample for the past few weeks. In a call with councilmembers on Friday, D.C. officials reported that Delta made up 1% of sampled positive cases over the past few weeks, but that Alpha remains the dominant strain in the region. (In a press conference earlier this week, DC Health director LaQuandra Nesbitt noted there are some limitations on sequencing, for example, only PCR tests can be sequenced, but antigen or “rapid” tests cannot be.) The city’s health department plans to update its online dashboard next week with variant cases and vaccine “breakthroughs,” where an immunized individual contracts coronavirus.
Relative to other parts of the U.S. with lower vaccination rates, and compared to the case counts recorded during the region’s winter surge, the slight increase in the area’s infections still remains quite low, and vaccines remain highly effective against the Delta variant.
But Nuzzo says that if nothing changes, the virus will continue to circulate in pockets and communities, giving it more opportunities to mutate into a strain that could potentially evade vaccines.
“I think what makes me concerned is seeing what’s playing out in other states. This virus is taking advantage of those pockets of susceptibility where they’re having, you know, fairly large increases in cases, predominantly among the unvaccinated,” Nuzzo said. “I think that should be a warning for any place that has people that are eligible for vaccines that aren’t getting vaccinated, we should really be making sure we’re going out to the communities offering vaccines as easily, and as excessively as possible, and really promoting its value.”
In D.C., the city has multiple vaccine incentives, like lotteries and freebie giveaways to promote vaccinations, especially in wards 7 and 8, which have reported the lowest rates of vaccinations in the city since the rollout began. As of June 16, roughly 33% of adult residents in Ward 8 have been fully vaccinated, compared to 54% in Ward 3. Larger gaps are appearing among younger residents, and the disparities don’t seem to be narrowing. About 5% of kids ages 12-15 in Ward 8 are fully vaccinated, compared to 53% of their peers in Ward 3.
In the Friday call with councilmembers, senior D.C. Health deputy Patrick Ashley stressed the importance of vaccinations, expecting that the number of confirmed cases of the Delta variant in D.C. will grow over the coming weeks.
“I think the key message here, and we can’t say this enough, and it gets to be the same story over and over again, but we need people to get vaccinated,” Ashley said.
Elliot Williams contributed reporting.
 Colleen Grablick
Colleen Grablick